Understanding Concussions
Each year, thousands of Marylanders seek emergency medical care for concussions—many of whom are young athletes injured while playing sports like lacrosse, soccer, baseball, basketball, and football. With the spring sports season just around the corner, it is critical that athletes, parents, and coaches make concussion prevention a priority.
In short, a concussion is a complex disturbance of brain function. While concussions are often considered “mild” traumatic brain injuries, their effects can be serious and can result in physical, cognitive, emotional, and sleep-related symptoms that can become permanent if not managed appropriately. Concussions do not always require a loss of consciousness or even a dramatic hit to the head; a simple “ding” or jolt can cause the brain to move rapidly within the skull and trigger a chain of neurological effects. Because symptoms can be subtle or delayed, athletes may not immediately recognize they have sustained a concussion. Many athletes’ concussions go undiagnosed, and if the head is hit again before full healing occurs, they risk long-term brain damage.
As the supervisor for the Injury Prevention Program at the R Adams Cowley Shock Trauma Center – with a decade of experience as a licensed physical therapist – I’ve seen firsthand the devastating effects of head injuries in young people. While the immediate symptoms of a concussion may seem insignificant, the long-term impact of a serious brain injury is anything but. According to Dr. Gary Schwartzbauer, Medical Director of the Neurotrauma Critical Care Unit at Shock Trauma, the “long-term consequences of traumatic brain injury not only impact the individual but also have implications for the family and community providing chronic supportive care,” thus underscoring why proper education and prevention are key.
SHOCK TRAUMA’S EXPERTISE IN NEUROTRAUMA CARE
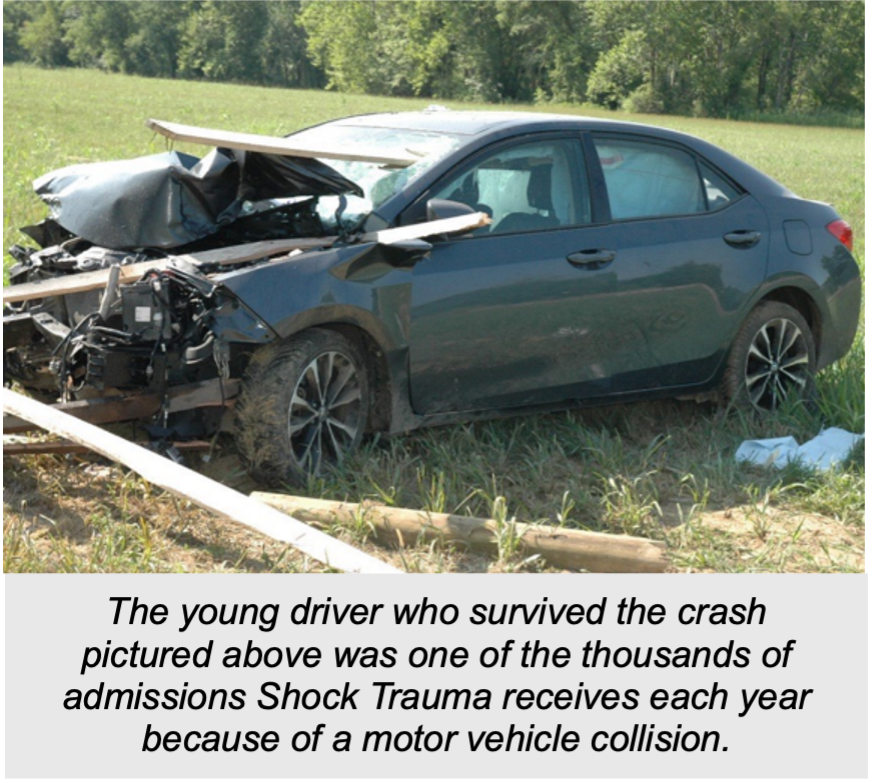
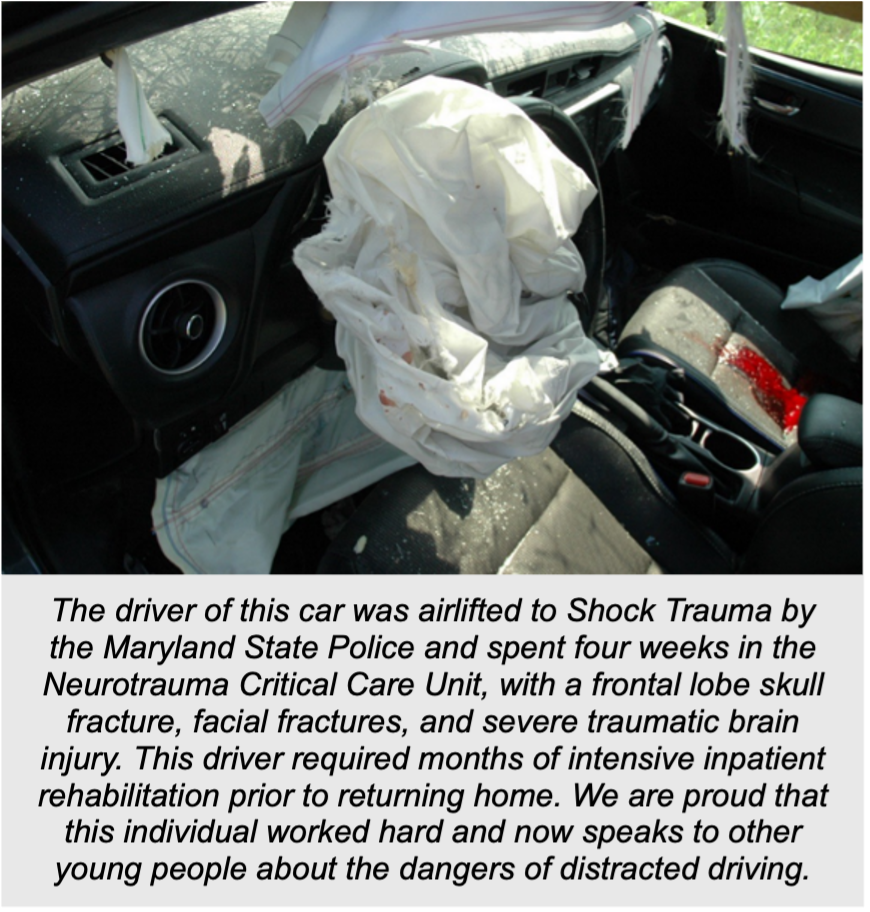
Shock Trauma is Maryland’s designated referral center for neurotrauma, an accreditation granted by the Maryland Institute for Emergency Medical Services Systems (MIEMSS). More than half of all patients treated at Shock Trauma experience some degree of trauma to the neurological system, and as such, Shock Trauma is both a state and national leader when it comes to complex neurotrauma care and research.
To provide these patients with the best, life-saving care, our neurosurgeons at Shock Trauma are available 24 hours a day and seven days a week for surgical intervention and consultation. Our specialized neurotrauma units provide high-level, multidisciplinary care to patients who have sustained these types of injuries. We can accommodate up to 36 neurotrauma patients between two units, some of whom are critically ill and require continuous monitoring and specialized neurocritical care. Many have otherwise undergone complex neurosurgical interventions, including placement of drains or tubes directly in the brain for monitoring, or surgical removal of part of the skull – sometimes replaced, and sometimes left off for healing.
THE CALL FOR PREVENTION: A PERSONAL PERSPECTIVE
Injury prevention spans a wide range of topics—driving safety, falls reduction, bleeding-related mortality prevention, and violence prevention—but of all the programs offered by the Shock Trauma Center for Injury Prevention and Policy, concussion prevention remains one of the least requested, despite being one of the most needed. Through my injury prevention work at Shock Trauma, I’ve worked extensively on outreach initiatives aimed at reducing preventable injuries, yet I continue to see a troubling gap when it comes to concussions: many adolescents still do not take concussions seriously. But a concussion is a brain injury, and without proper care, it can have serious consequences.
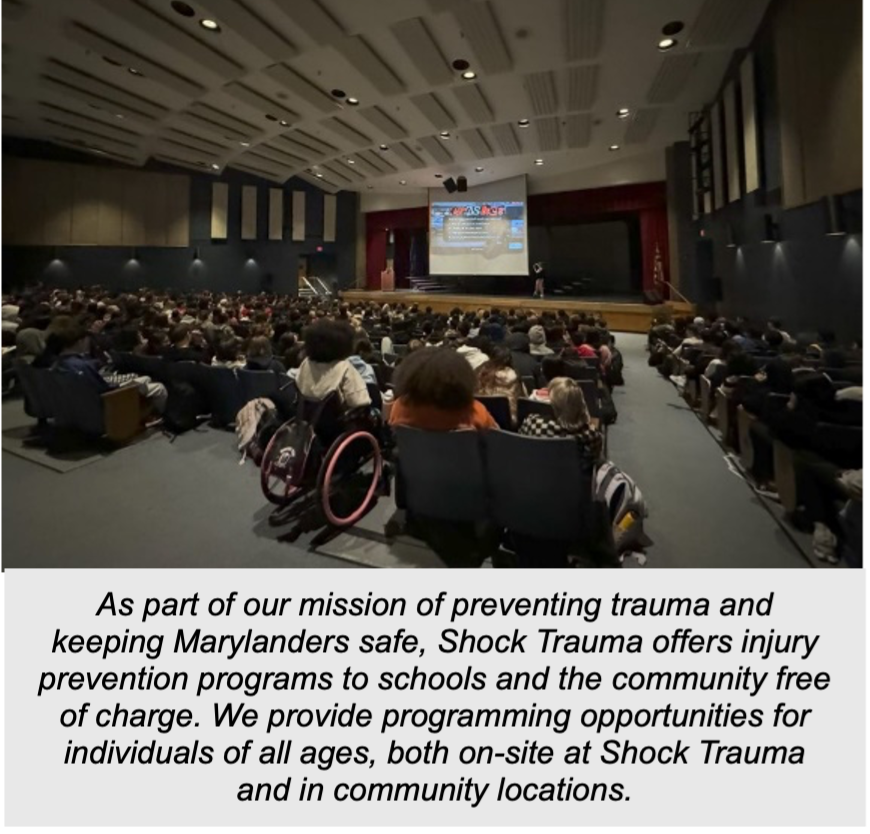
Since the establishment of our partnership with the ThinkFirst National Injury Prevention Foundation about two years ago, my team has worked to bridge this gap through our concussion prevention program, delivering educational programs to more than 25 different groups and reaching more than 700 individuals. In my personal experience, the most significant part of our program is what I consistently observe to happen at the conclusion of the program. Students tend to discreetly approach me with questions about their own past head injuries — injuries they had previously brushed off, played through, or ignored. Many describe instances where they experienced dizziness, difficulty concentrating, or persistent headaches, but had not previously recognized these symptoms as being serious until participating in our program. Their concerns, often unvoiced until informed by the knowledge from our program, reinforce just how much prevention education is needed.
IDENTIFY, MANAGE, PREVENT
The quick identification of a concussion is essential for proper treatment and recovery. The trouble lies in the fact that sometimes symptoms appear immediately, but sometimes they develop gradually hours or even days after an injury. Common physical symptoms include headaches, dizziness, nausea, vomiting, sensitivity to light and sound, balance issues, and blurred or double vision. Cognitive and emotional symptoms may include confusion, irritability, difficulty concentrating, memory problems, mood swings, or other unusual emotional responses. Many individuals describe feeling groggy, foggy, sluggish, or simply “not quite right.” Sleep disturbances are also common, such as sleeping more or less than usual or having difficulty falling or staying asleep. Just one of these symptoms is enough to diagnose an individual with a concussion.
Concussion symptoms should never be ignored or concealed. If there is any suspicion of a concussion following a blow or jolt to the head, the very first thing to do is remove yourself from all activity and get checked out. Any activity that could potentially cause further head trauma must be completely avoided, as a second-impact injury to an injured brain can lead to permanent damage and even death. Management typically involves a combination of rest, symptom monitoring, and time, as the brain needs a chance to heal. During this recovery period, both physical and mental rest are essential. This includes limiting screen time, avoiding physical activities, and getting adequate sleep. Once an individual is completely symptom-free and has been cleared by a doctor, a gradual return to activity is allowed, starting with light tasks and consciously reintroducing activities under medical supervision.
The best way to manage a concussion is to prevent it from happening in the first place. Start by using proper equipment, including helmets and other protective gear designed for your specific activity. Ensure that helmets fit correctly and are worn properly, and remember – while a helmet will significantly reduce the severity of a head injury, it may not always prevent a concussion. Your skull and brain are fragile, and since a helmet will only do so much, physical conditioning and good technique are also key. Adhere to safety guidelines, avoid unnecessary force, and follow the directives of your coach. Respect the game’s regulations, which are put into place with player safety in mind. Fostering a culture of safety within teams, schools, and peer groups is of utmost importance. When brain health is valued and personal safety is prioritized, adolescents are more likely to make smart choices that help keep them safe.
———————-
Dr. Kristin Barron has been with Shock Trauma as a physical therapist since 2015. She developed a passion for supporting individuals with critical illnesses and traumatic injuries through her extensive experience working on the hospital’s critical care units, including the neurotrauma ICU and the multi-trauma ICU. She now serves as the supervisor for the Shock Trauma Injury Prevention Program, where she leads and coordinates trauma prevention outreach programs throughout the state. Additionally, Kristin oversees the Trauma Survivors Network at Shock Trauma, where she thrives on creating opportunities that connect the worlds of trauma prevention and trauma survivorship.